MENINGITIS
Incidence
Anaerobic bacteria are rarely the cause of acute bacterial meningitis1,2 Because cultures of cerebrospinal fluid (CSF) for anaerobes rarely are done, the rate of anaerobic meningitis could be higher.
Microbiology and pathogenesis
The predominant anaerobes causing meningitis are Gram-negative bacilli ( including Bacteriodes fragilis group ), Fusobacterium spp. (mostly Fusobacterium necrophorum) and Clostridium spp. (mostly Clostridium perfringens).1,2 Peptostreptococcus spp., Veillonella, Actinomyces, Propionibacterium acnes and Eubacterium are less commonly isolated. The main predisposing conditions to anaerobic meningitis are: ear nose & throat infections gastrointestinal disease, and skull fractures. Less common causes are: skull trauma, lumbar puncture, head and neck neoplasm, congenital dermal sinuses, meningorectal fistulae, ventricular shunts, pulmonary disease, peritonitis, and, pilonidal cyst abscesses. 1-3 Meningitis caused by Fusobacterium necrophorum has been associated with chronic otitis media and an episode of upper respiratory infection. 4,5
Shunt infection with Propionibacterium spp. was reported, especially in association with ventriculo-auricular and ventriculo-peritoneal shunts. This organism is also found in 25% of post intrcranial surgery.5a Anaerobic meningitis is generally monomicrobial and is less likely to be a mixed anaerobic-aerobic infection. Multiple organisms mostly B. fragilis and Enterobacteriaceae were reported in meningitis complicating dermal sinus tract infection5 and ventriculo-peritoneal shunt infections following perforation of the gut by the shunt’s distal tube.6 C. perfringens is a cause of meningitis following head injuries or surgery,2,7 that is fatal in about a third of patients despite therapy.
Diagnosis
The symptoms, signs and laboratory findings associated with meningitis caused by anaerobic bacteria do not generally differ from those associated with other bacteria. Patients can present with headache, vomiting, stiff neck, lethargy, or irritability and fever.
Clues to the presence of meningitis caused by anaerobic bacteria are the absence of bacterial growth in routine cerebrospinal fluid (CSF) cultures in the face of findings suggesting bacterial infection. These include: the presence of bacteria on Gram stain, elevated neutrophil count, and protein and a reduced glucose concentration. The presence of more than one bacterial strain in Gram stain and the ability to grow only one isolate is another indication. Patients who fail to respond to appropriate antimicrobial therapy should be examined for the presence of anaerobes because of the possibility of mixed aerobic and anaerobic infection.36
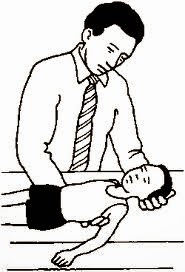
Stiff neck in meningitis
Meningitis caused by anaerobes should be suspected especially in clinical predisposing situations, such as chronic otitis media and sinusitis, mastoiditis, dental abscess, anaerobic bacteremia, following perforation of an abdominal viscus, following surgery, and head trauma. Special consideration should be given to newborns at high risk to develop anaerobic infection, especially those who were born to mothers with amnionitis or in meningitis in a compromised neonate.
Because of the association between subdural or epidural empyema and brain abscesses with meningitis, the presence of such abscesses warrants excluding possible concurrent meningitis.
Management
Most Gram-positive anaerobes are susceptible to penicillins. However, many Gram-negative anaerobes resist these antibiotics, and therefore susceptibility testing is necessary to ensure proper therapy.8 These organisms are generally susceptible to several antimicrobials that penetrate the CSF, including metronidazole, chloramphenicol, ticarcillin and the carbapenems (i.e. meropenem). Imipenem has been associated with an increase rate of seizures in those with CNS disorders or renal dysfunction. Clindamycin and cefoxitin are not recommended in CNS infections because of their poor penetration into the CSF.
Some of the newer quinolones (ie trovafloxacin) that are effective against anaerobes, may be effective in the therapy of anaerobic meningitis.8 Metronidazole is very active in vitro against Gram negative anaerobes and achieves high levels in CSF. P. acnes and other Gram-positive anaerobes are generally resistant to metronidazole.
The length of antimicrobial therapy depends on the patient’s response and underlying illness. It should be given for at least 14 days.
In patients with mixed aerobic and anaerobic CNS infection, antimicrobial coverage against all organisms present is necessary. Because metronidazole is effective only against anaerobic organisms, additional coverage for the other organisms should be added in instances of mixed infection. Complete eradication of the organisms in the CSF may be difficult when insufficient antimicrobial agents penetrate into the cerebrospinal fluid. Repeated spinal tap would ensure eradication of the organisms and allows measurement of concentration of the antimicrobial agents in the CSF. Elimination of associated foci of infection is crucial. Failure to drain inflamed foci adjacent to the CSF can prevent complete cure.
P. acnes shunt infection is treated with antimicrobials and when needed- shunt removal. In cases of ventriculo-peritoneal shunt infections after perforation of the colon, surgical repair of the perforation as well as removal of the shunt is necessary.7
INTRACRANIAL ABSCESSES
Intracranial abscesses can be classified as brain abscesses or subdural or extradural empyema. Brain abscess is an uncommon but serious life-threatening infection. It can originate from infection of contiguous structures, such as chronic otitis media and sinusitis, dental infections, mastoiditis, as the result of hematogenous spread from a remote site, after skull trauma or surgery; or following meningitis.
Microbiology
The predominant organisms causing brain abscesses are aerobic and anaerobic Streptococcus spp. ( Peptostreptococcus spp. and microaerophylic streptococci, isolation frequency of 60%–70%), Gram-negative anaerobic bacilli (Bacteroides fragilis group , Prevotella spp., Porphyromonas spp. and Fusobacterium spp., 20%–50%), Enterobacteriaceae (20%–30%), S. aureus (10%–15%), and fungi (10%–15%) 10
Yeast and fungi predominate in immunocompromised patients and those with cancer. These include Aspergillus sp., Candida spp., Cryptococcus neoformans, Coccidioides immitis and the mucormycosis agents. Protozoa and helminths may also cause brain abscess. These include Entamoeba histolytica, Cysticerosis, Schistosoma japonicum, and Parogonimus spp.11 Patients with T- lymphocyte defects and those with AIDS are susceptible to Toxoplasma gondii, Nocardia asteroides, Mycobacterium spp., Listeria monocytogenes, Enterobacteriaceae, and Pseudomonas aeruginosa.
Pathogenesis
Anaerobes can spread from contiguous sites of existing infections resulting in epidural or cerebral abscesses, subdural empyema, or septic thrombophlebitis of the cortical veins or venous sinuses.12
Infection may enter the intracranial compartment by: (1) Direct extension throught necrotic areas of osteomyelitis, after trauma that caused open fracture or following neurosurgery. Contiguous spread could extend to various sites in the CNS , causing cavernous sinus thrombosis, retrograde meningitis, and epidural, subdural,and brain abscess.12 (2) Spread through the valveless venous systems that connects the intracranial and the sinus mucosal veins ( common in sinusitis). (3) Haematogenic spread from a distant focus.
The site of the primary infection or the underlying condition can determine the etiology of the brain abscess. Anaerobic Gram-negative anaerobic bacilli are commonly recovered in association with ear and sinus infections.1 Spread by blood usually originate in the lung. Anaerobic and microaerophilic streptococci, as well as streptococci viridans, are common in abscesses associated with congenital heart disease. Enterobacteriaceae and anaerobes may spread from intraabdominal or genitourinary sites.1 S. aureus is commonlly isolate following trauma and neurosurgical procedures. Dental infections can spread into the CNS via the sinuses.
Clinical manifestations
Brain abscess is usually manifested by fever and symptoms of a space-occupying lesion. These include persistent localized headache, drowsiness, confusion, and stupor, general or focal seizures, ataxia nausea and vomiting, and focal motor or sensory impairments. Localized neurologic signs are often found eventually. In the initial stages the infection is in a form of encephalitis accompanied by signs of increased intracranial pressure such as papilledema. A ruptured brain abscess may produce purulent meningitis.
Brain abscess
Diagnosis
Cultures for aerobes, anaerobes, acid-fasts, fungi and stainings should be obtained whenever possible; with the assistance of CT-guided needle if necessary. The opening pressure of the CSF generally is elevated. If the diagnosis of intracranial suppuration is suspected, a lumbar puncture (LP) should be deferred to avoid brain herniation. MRI or CT can evaluate the presence of brain abscess prior to LP. The usual CSF findings associated with subdural or parenchymal abscesses consist of an elevated protein, pleocytosis with a variable neutrophil count, a normal glucose, and sterile cultures. The number of white blood cells and red blood cells is elevated when the abscess ruptures.
Skull films can be important in the diagnosis of sinusitis or the presence of free gas in the abscess cavity. Electroencephalogram occasionally can reveal a focus of high voltage with slow activity; however, this is the least accurate procedure in the diagnostic evaluation. MRI is the diagnostic and follow-up method of choice and permits diagnosis and follow-up of the lesions as compared to CT. Since the advent of CT and MRI scanning, the case fatality rate has fallen by 90%.13
Brain abscess CT
Management
Medical care: Before encapsulation antimicrobials therapy accompanied by intracranial pressure control are essential and may prevent abscess formation. Once an abscess has formed, surgical excision or drainage combined with a long course of antibiotics (4 to 8 weeks) is necessary. Some neurosurgeons advocate complete abscess evacuation while others advocate repeated aspirations.14 In cases with multiple abscesses or in those with abscesses in essential brain areas, repeated aspirations are preferred to complete excision.14
CT-guided needle aspiration may provide the etiological agent(s). Frequent scans, at least once a week, are essential in monitoring treatment response. Although surgical intervention remains essential, selected patients may respond to antibiotics alone.14
The corticosteroids use is controversial. Steroids can retard the encapsulation process, increase necrosis, reduce antibiotic penetration into the abscess and alter CT images. Steroid therapy can also produce a rebound effect when discontinued. When used to reduce cerebral edema, therapy should be for a short duration. The appropriate dosage, the timing and their effect on the course of the disease are unknown.14
The antimicrobial treatment of the brain abscess is generally long. However, a shorter course can be given if surgical drainage is achieved. Because of the difficulty involved in the penetration of various antimicrobial agents through the blood-brain barrier, the choice of antibiotics is restricted.
Initial empiric antimicrobial therapy should be based on the expected etiological agents according to the likely primary infection source. Penicillin penetrates well into the abscess cavity and is active against non-beta lactamase producing anaerobes and aerobic organisms. Chloramphenicol penetrates well into the intracranial space, and is active also against Haemophilus spp., and most obligate anaerobes. Metronidazole penetrates well into the CNS , but is only active against strict anaerobes. Third-generation cephalosporins (i.e., cefotaxime, ceftazidime) are generally adequate therapy of aerobic Gram-negative organisms. Aminoglycosides do not penetrate well into the CNS , and are relatively less active because of the anaerobic conditions and the acidic contents of the abscess. Beta-lactamase resistant penicillins (i.e., oxacillin) provide good coverage against S. aureus. However, their penetration into the CNS is less than penicillin. Vancomycin is the most effective against meticillin-resistant S. aureus and S. epidermidis as well as aerobic and anaerobic streptococci and Clostridium spp.
B. fragilis group and over half of strains of Prevotella spp., Porphyromonas spp. and Fusobacterium spp. resist penicillin. Agents effective against these organisms that penetrate the blood-brain barrier include metronidazole, chloramphenicol, ticarcillin plus clavulanic acid and the carbapenem (e.g. imipenem, meropenem). Caution should be used in administering imipenem, as high doses of this agent were associated with seizure activity. Therapy with penicillin should be added to metronidazole to cover aerobic and microaerophilic streptococci. The administration of beta-lactamase-resistant penicillin or vancomycin for the treatment of S. aureus is generally recommended. Whenever proper cultures are taken and organisms are isolated, the initial empiric therapy can be adjusted to specifically treat the isolated bacteria.
Surgical Care: Patients who do not meet the criteria for medical therapy alone, require surgery. Delay in surgical drainage and decompression can be associated with high morbidity and mortality. Two surgical approaches are available: steriotactic aspiration, and exision. Repeating aspiration may cause bleeding. Excision is indicated in posterior fosa or multiloculated abscess, and those that are caused by fungi or helmites, and those that reaccumulate following repeated aspirations.
REFERENCES
1. Finegold, S.M.: Anaerobic bacteria in human diseases. New York
, Press.
2. Law D A., Aronoff S C., .: Anaerobic meningitis in children; case report and review of the literature. Pediatr. Infect. Dis. J. 1992;11:968–71.
3. Aucher P., Saunier J.P., Grollier G. et al.: Meningitis due to Enterotoxigenic Bacteroides fragilis. Eur. J. Clin. Microbiol. Infect. Dis. 15:820–1996.
4. Jacobs, J.A., Hendriks, J..J.E., Verschure, P.D.M.M., et al.: Meningitis due to Fusobacterium necrophorum subspecies necrophorum: case report and review of the literature. Infection 21:57–60, 1993.
5. Brook, I. : Anaerobic meningitis in an infant associated with pilonidal cyst abscess. Clin. Neurol. Neurosurg. 87:131, 1985.
6. Brook, I. , Johnson N, Overturf GD, Wilkins J..: Mixed bacterial meningitis: a complication of ventriculo and lumboperitoneal shunts. Report of two cases. J. Neurosurg. 47:961, 1977.
7. Debast, S.B., van Rijswijk, E., Jira, P.E., Meis, J.F.: Fatal Clostridium perfringens meningitis associated with insertion of a ventriculo-peritoneal shunt. Eur. J. Clin. Microbiol. Infect. Dis. 12:720–1, 1993.
8. Lutsar, I. , McCracken, G.H. Jr., Friedland, I.R.: Antibiotic pharmacodynamics in cerebrospinal fluid. Clin. Infect. Dis. 27(5):1117-27, 1998.
9. Rasmussen, B.A., Bush, K., Tally, F.P.: Antimicrobial resistance in anaerobes. Clin. Infect. Dis. Suppl 1:S110–20, 1997.
10. Brook, I. : Anaerobic and anaerobic microbiology of intracranial abscess. Pediatric. Neurology. 8:210–214, 1992.
11. Hagensee , M.E.
12. Lerner, D.N., Choi, S.S., Zalzal, G.H., Johnson, D.L.: Intracranial complications of sinusitis in childhood. Ann. Otol. Rhinol. Laryngol. 104(4 Pt 1):288–93, 1995.
13. Wong, J., Quint, D.J.: Imaging of central nervous system infections. Semin Roentgenol 34(2):123–43, 1999.
14. Townsend, G.C., Scheld, W.M.: Infections of the central nervous system. Adv. Intern. Med. 43:403–47, 1998.