5. American Academy of Pediatrics. Tetanus (lockjaw).Pickering L K editor. 2009;665-660. Red Book: Report of the Committee on Infectious Diseases, 28th ed. Elk Grove Village, IL: American Academy of Pediatrics; 2009.
BOTULISM
Botulism is caused by a neurotoxin produced from the anaerobic, spore-forming bacterium Clostridium botulinum. Botulism in humans is usually caused by toxin types A, B, and E.
These are forms of botulisms: food-borne botulism, wound botulism, infant botulism, adults intestinal toxemia botulism, inhalation botulism, unclassified botulism (in patients over 12 month old with proven botulism without an ingestion source), and iatrogenic botulism. Symptoms and pathologic findings relate to the toxin’s effects on the nervous system and are characterized by neuromuscular dysfunction and resultant flaccid paralysis of muscles.
FOOD-BORNE BOTULISM
Epidemiology
Food-borne botulism, the most common form of botulism, usually occurs in small sporadic outbreaks.1 Botulism toxin is the most dangerous toxin known, as only 0.5 g of toxin A is lethal for humans. The toxin is ingested with food that has become contaminated with C. botulinum during canning or other preparatory process.1
C. botulinum spores are highly heat-resistant; they may survive several hours at 100°C; however, exposure to moist heat at 120°C for 30 minutes will kill the spores. The toxins, on the other hand, are destroyed by heat, and cooking food at 80°C for 30 minutes safeguards against botulism.1 As a result, the ingestion of preformed toxin, not simply spores, is required in adult botulism. In infant botulism, however, the toxin can be produced by incubation of the spores within the gut.2
Most U.S. outbreaks of botulism are associated with food products that are not heated adequately before consumption and in which spores form toxins. In the United States, preserved foods in which the toxin is most commonly found include string beans, corn, mushrooms, spinach, olives, onions, beets, asparagus, seafood, pork products, and beef.2,3 Improperly smoked or canned fish is the source of type E intoxications. Botulinum spores are common in soil, dust, lakes, and other environmental matter and can contaminate fruits, vegetables, meats, and fish. Honey has become recognized as a potential source of C. botulinum spores and one of the botulism.
Canned food contaminated with Clostridium botulinum
The causative agent is one of several eight closely related serologically toxins elaborated by the sporulating, C. botulinum. Human poisoning usually is caused by type A, B, or E toxin, rarely by type C1, C2, D, F or G.4
Three steps are necessary for toxin-induced neuromuscular blockade: (a) transport across the intestinal wall into the serum, (b) binding to neuronal receptors, and (c) internalization of bound toxin, an irreversible step leading to impairment of neurotransmitter release and resultant neuromuscular blockade.4
Botulinal toxin type A has therapeutic value in the therapy of a several neurologic and ophthalmologic disorders through chemical denervation.5 They are used as a therapeutic agent through local instillations in strabismus, blepharospasm, and other facial nerve disorders.
Clinical findings
There are four cardinal clinical features of botulism6:
1. Symmetric and descending neurologic manifestations.
2. Intact mental processes.
3. No sensory disturbances, although vision may be impaired because of extraocular muscle involvement.
4. Absence of fever unless secondary infectious complications occur.
At 18 to 48 hours after ingestion of tainted food, patients present with cranial nerve dysfunction manifested by diplopia, dysphagia, and difficulty in speaking. They remain lucid, although anxiety and agitation may develop. Additional signs may include pupillary dilation, vertigo, tinnitus, and dry mouth and mucous membranes. The descending progression of paralysis in botulism occurs at various rates, spreading and involving muscles of respiration and most voluntary musculature. The major manifestation is respiratory embarrassment, which may appear gradually or suddenly. 2,6
Involvement of the gastrointestinal tract varies and is related somewhat to the toxin serotype. Types A and B, cause abdominal complaints (e.g., abdominal pain, bloating, cramps, diarrhea) in approximately one-third of patients that are replaced quickly by constipation. Type E produces more significant gastrointestinal complaints than do the other types. 2,6
The chief cause of mortality is respiratory or bulbar paralysis. The typical duration of symptoms exceeds 1 month, and full recovery from weakness and fatigability may require as long as 1 year.
Diagnosis
Diagnosis is suggested by the pattern of neuromuscular disturbances and a likely food source and is confirmed by demonstration of botulinus toxin or C. botulinum in suspected food, vomitus, and serum. Electromyography (EMG) can be helpful in diagnosis when lowered amplitude action potentials following low-frequency stimulation and posttetanic facilitation of the muscle action potential can be demonstrated.
The isolated muscle action potential is reduced, but repetitive nerve stimulation results in facilitation of the action potentials.
Suspected cases must be reported to local and state health authorities and to the Center for Disease Control and Prevention (tel. 800-232-4636), from which trivalent antitoxin for types A, B, and E is available. Blood and stool samples should be transported to a laboratory (usually state health departments) equipped to determine botulinal toxin. Stool should be cultured for Clostridium because C. botulinum . Definitive diagnosis can be made by demonstration of preformed toxin by the mouse inoculation test.
Botulism may be confused with poliomyelitis, viral encephalitis, myasthenia gravis, Guillain-Barré syndrome, tick paralysis, and atropine or mushroom poisoning.
Management
Mortality rate has dropped from 60% to 16%, most likely a result of improvement in critical care management. The longer incubation period, the better is the prognosis.
Management involves optimal supportive care and specific therapy directed at neutralizing unbound toxin, eradicating any infection with C. botulinum and management of secondary infections. Speed is essential in diagnosis so that circulating toxin can be neutralized before it binds to nerve endings. Induced vomiting and gastric lavage is carried out if exposure has occurred within several hours. Bowel purges have been suggested. Airway control, proper oxygenation and management of adequate ventilation is of great importance. Endotracheal intubation may be required. 7
Oral or parenteral antimicrobials such as penicillin have limited value but may destroy some viable C. botulinum organisms. Aminoglycosides can affect the neuromuscular junction and potentiate the effect of botulinal toxin and should be avoided.
The administration of appropriate antitoxin without delay is recommended. It has little effect with types A and B and a greater effect with type E toxin poisoning. Several forms of equine botulism antitoxin are available: monovalent type E, bivalent AB, trivalent ABE, and polyvalent ABCDEF. If the causative toxigenic type is unknown, or if type-specific antitoxin is not available, the trivalent ABE preparation should be used. 7
If hypersensitivity to horse serum is not demonstrated, the antitoxin can be given intravenously at a dose of one vial every four hours for a total of four or five vials. If toxin is still detectable in subsequent serum samples, additional antitoxin may be given after repeat skin testing. Guanidine may enhance the release of acetylcholine from nerve terminals and may help in mild cases; however, guanidine is less effective in overcoming respiratory muscle paralysis.
Prevention
Prevention is of utmost importance. Proper home and commercial canning and adequate heating of food before serving are essential. Food showing any evidence of spoilage should be discarded. After a case has been recognized, health authorities must be notified so that other potential cases can be identified and treated expectantly.
WOUND BOTULISM
Epidemiology
Wound botulism is rare in the USA. Most cases involve wounds located on an extremity.
Predisposing factors
Wound botulism is associated with major soil contamination through compound fractures, severe trauma, lacerations, puncture wound, “skin popping” of black tar heroin, and hematoma.7
Etiology
The pathogenesis and etiology of wound botulism are similar to the food-borne disease. Most wound cases have been associated with type A toxin-producing organism, and some with type B.
Clinical signs and diagnosis
The incubation period is longer (4 to 18 days) than for food-borne illness (six hours to eight days). The clinical manifestations are similar to those of food-borne botulism except for the lack of early gastrointestinal symptoms. The wound can look benign, with minimal erythema, induration or discharge, but the organism and toxin are usually present.2
The lesion is unroofed to obtain specimens for culture and toxin assay. Diagnosis is confirmed by EMG and demonstration of toxin in serum or by isolation of C. botulinum and/or toxin from the wound in association with appropriate clinical findings.
Management
Treatment of wound botulism must include debridement, drainage, and wound irrigation. Good supportive care, as previously described, primarily respiratory support, is also an important aspect of management. Although antitoxin will not improve paralysis from toxin already bound at the neuromuscular junction, antitoxin will bind circulating toxin.
Adult intestinal toxemia botulism
Adult intestinal toxemia botulism occurs rarely and sporadically and results from of absorption of toxin produced in situ by botulinum-toxin producing Clostridia that colonizes the intestine. Generally, patients have an anatomical or functional bowel abnormality or are using antimicrobials, which may select fastidious Clostridia species from the normal bowel flora. 8-11 The symptoms may be protracted and relapse even after treatment with antitoxin because of the ongoing intraluminal production of toxin. Typically there is no known food or wound source and prolonged excretion of organisms and toxin are present in the stool.
Inhalational botulism.
Inhalational botulism is iatrogenic and was described only once among laboratory workers in 1962, with symptoms similar to foodborne botulism. 12 Deliberate dissemination of botulinum toxin by aerosol is a potential biological weapon could produce an outbreak of inhalational botulism. 13
Iatrogenic botulism
Iatrogenic botulism occurs after injection of botulinum toxin for therapeutic or cosmetic purposes. The doses recommended for cosmetic treatment are too low to cause systemic disease. However, higher doses injected for treatment of muscle movement disorders have caused systemic botulism-like symptoms in patients. 13 Injection of highly concentrated botulinum toxin have caused severe botulism in some patients who received it for cosmetic purposes.
Iatrogenic botulism was reported in four patients who received botulinum toxin injections using an unlicensed, highly concentrated preparation of botulinum toxin A. 14 The patients received doses as high as 2857 times the human lethal dose by injection and had serum toxin levels 21 to 43 times the estimated lethal human dose by injection. All patients survived following administration of equine serum antitoxin, and required prolonged mechanical ventilation and physical rehabilitation.
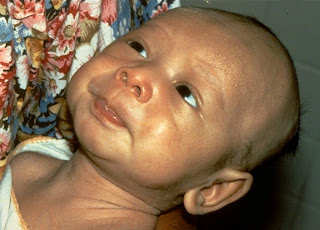
INFANT BOTULISM
Infant botulism occurs as a result of absorption of the heat labile neuro-toxin that is produced by that colonizes the intestinal tract of an infant younger than one year. It is an age limited neuro-muscular illness that is different from the classical illness in that the toxin is generated by the organisms in the infant's intestine, the thereafter absorbed to produce the illness.
The organisms generally are squired from the environment and include honey and soil. Clinical manifestations are caused by progressive neuromuscular blockage, starting with muscle innervated by the cranial nerves and than the trunk, extremities and the diaphragm. The presynaptic autonomic nerves are also effected.
Diagnosis is based on clinical presentation and confirmed by by detection of the toxin or isolating the organism from stool. Management included supportive intensive care which includes mechanical ventilation and administration of human botulism immunoglobulin in severe cases.15
An infant with botulism
REFERENCES
1. Hatheway, C.L. Botulism: the present status of the disease. Curr Top Microbiol Immunol 195:55–75, 1995.
2. Ferrari, N.D., 3rd, Weisse, M.E.: Botulism. Adv Pediatr Infect Dis 10:81–91, 1995.
3. Shapiro, R.L., Hatheway, C., Swerdlow, D.L.: Botulism in the United States: a clinical and epidemiologic review. Ann Intern Med 129:221–8, 1998.
4. Brin, M.F. Botulinum toxin: chemistry, pharmacology, toxicity, and immunology. Muscle Nerve Suppl 6:S146–68, 1997.
5. Jankovic, J., Brin, M.F.: Therapeutic uses of botulinum toxin. N Engl J 324:1186–94, 1991.
6. Cherington, M.: Clinical spectrum of botulism. Muscle Nerve 21:701–10, 1998.
7. Robinson RF, Nahata MC. Management of botulism. Ann Pharmacother. ;37:127-31, 2003.
8. Chia JK, Clark JB, Ryan CA, Pollack M. Botulism in an adult associated with food-borne intestinal infection with Clostridium botulinum. N Engl J Med. 1986; 315:239 54.
54.
9. Arnon S. Botulism as an intestinal toxemia. In: Blaser MJ, Smith PD, Ravdin JI, Greenberg HB, Guerrant RL, ed. Infections of the gastrointestinal tract. New York: Raven Press, 257 71,1995
71,1995
10. Fenicia L, Franciosa G, Pourshaban M, Aureli P. Intestinal toxemia botulism in two young people, caused by Clostridium butyricum type E. Clin Infect Dis. 29:1381 7,1999.
7,1999.
11. Griffin PM, Hatheway CL, Rosenbaum RB, Sokolow R. Endogenous antibody production to botulinum toxin in an adult with intestinal colonization botulism and underlying Crohn's disease. J Infect Dis. 175:633-7, 1997.
12. Middlebrook JL, Franz DR. Botulinum toxins. In: Sidell FR, Takafuji TE, Franz DR, eds. Medical aspects of chemical and biological warfare. Washington, DC: Borden Institute, Walter Reed Army Medical Center, 643: 54,1997.
14. Chertow, DS, Tan, ET, Maslanka, SE, et al. Botulism in 4 adults following cosmetic injections with an unlicensed, highly concentrated botulinum preparation. JAMA 2006; 296:2476-9.
15. Long S. S. Infant botulism. Pediatr Infect Dis J. 2001;20:707-9.